Investments in public health programs appear to reduce spending in the Medicare program, providing an economic benefit for seniors and the federal budget as growing numbers of baby boomers join Medicare. Results from a new study published in the December issue of the journal Health Services Research by our research team at the University of Kentucky suggest new directions for containing costs by aligning medical and public health programs.
Public health programs aim to prevent diseases and injuries within the public at large, such as those caused by tobacco smoke, poor nutrition, inadequate physical activity, contaminated food and water, or exposure to infectious diseases like influenza. Logic dictates that these programs, if effective, may reduce the need for costly medical care, particularly as people age and accumulate health problems. But research confirming the existence and the size of this effect, which economists and policy analysts call a medical cost offset, has not been available until now.
Estimating Public Health’s Medical Cost Offsets
The new study tracks hundreds of U.S. communities over the period 1993-2013. We measured the amount of money spent annually by local public health agencies in each community, and linked these data with measures of Medicare spending per beneficiary in the same local areas, along with detailed information on demographic, economic and community characteristics. Using an advanced statistical methodology known as instrumental variables analysis, we estimated how public health spending influenced Medicare spending over time, while controlling for other factors that tend to obscure the true causal relationship between these two types of spending.
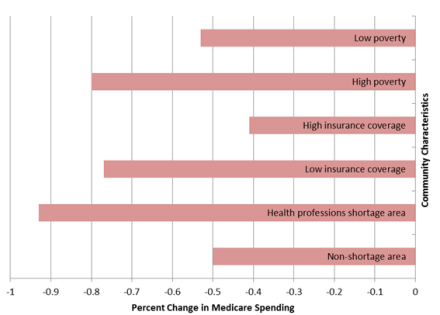
The results show that Medicare spending per beneficiary fell by about 1 percent for each 10 percent increase in public health spending per resident, with larger offsets observed in low-income and medically underserved communities. These findings suggest that the federal Medicare program could realize an average of $1.10 in savings for each $1.00 invested in local public health activities over time.
Figure: Estimated Impact of a 10% Increase in Public Health Spending Per Capita
Implications for Policy and Practice
A large body of research examines the causes and consequences geographic variation in Medicare resource use – work led by scholars at Dartmouth and elsewhere. Most of the empirical research has focused on supply-side factors and, to a lesser extent, patient preferences. This study is the first to suggest that public health programs and resources may contribute to this variation in important ways.
Local public health agencies appear to generate important but largely hidden economic benefits for their communities, alongside the more visible health benefits. Consequently, medical providers who participate in Medicare’s value-based payment models like accountable care organizations and shared-savings programs should explore the roles that public health agencies can play in helping to improve outcomes and contain costs.
One challenge highlighted by the study’s findings is the so-called “wrong pocket” problem that can undermine incentives to invest in public health programs. Many public health agencies are funded predominantly by state and local government contributions, but the Medicare savings generated by their work accrues to the federal government. Resolving this problem will require new models for public health financing, such as including public health agencies in Medicare’s shared savings models.
The study cannot rule out the possibility that other factors may contribute to the observed connection between public health spending and Medicare savings in local communities. For example, communities that choose to invest in robust public health programs may support other social and community resources that help to constrain Medicare spending, such as better housing and transportation options for seniors. Nevertheless, the study’s strong research design and analysis make this possibility less likely to affect the results.
For More Information
The study was conducted as part of the Robert Wood Johnson Foundation’s Systems for Action national research program, which studies new models for aligning the work of medical, social, and public health sectors in ways that improve health and wellbeing. The study appears in the December 2017 issue of Health Services Research, in a special theme issue featuring research on the economics of public health services. For more information, contact me at glen.mays@uky.edu